"Sample hemolysis is the most common error source in clinical laboratory and the main reason for sample rejection. The wrong result report due to sample hemolysis may lead to misdiagnosis and mistreatment, re blood drawing will increase the pain of patients, prolong the reporting cycle, and cause human, material and economic losses"
1) How to judge hemolysis?
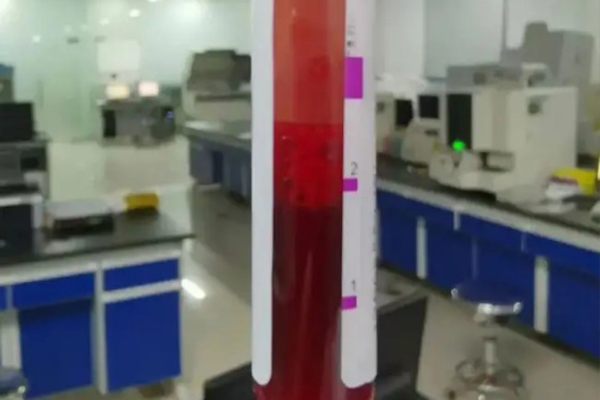
Generally, the sample after centrifugation is observed to judge whether it is hemolytic, but sometimes the sample is slightly red turbid due to careless vibration after centrifugation, which will also be regarded as hemolysis if it is not looked carefully. So, how can we determine whether it is true hemolysis? The best way is to measure the hemoglobin content in the serum, that is, the hemolysis index, to know whether there is hemolysis.
How to define whether the sample has clinical test related hemolysis? At present, the conventional method is to judge according to the hemolysis index (HI). Hemolysis index is actually the level of free hemoglobin in plasma. Some researchers compared 50 studies on hemolysis and found that 20 used hemolysis index to define hemolysis, 19 used visual inspection, and the other 11 did not indicate the method.
The practice of using visual hemolysis to choose clinical samples is considered inaccurate because of the lack of objective quantitative standards and the sensitivity of different indicators to hemolysis. In a study in cludia in 2018, people carefully followed up 495 blood samples and test results in the emergency room. It was found that visual judgment of hemolysis could lead to improper test results of up to 31%, including 20.7% of cases where hemolysis had an impact on the results but was ignored, and 10.3% of cases where the test results were suspended but later found not to be affected by hemolysis.
2) Causes of hemolysis
The causes of hemolysis can be divided into clinical examination related hemolysis and non clinical examination related hemolysis from the perspective of whether they are related to the clinical examination process. Clinical test related hemolysis refers to hemolysis caused by red blood cell rupture due to improper clinical test operation, which is the focus of our discussion. Clinical practice and relevant literature have proved that the occurrence of hemolysis is directly related to the sample collection process. In the process of clinical examination, hemolysis will be caused if the caliber of blood collection needle is too small, the blood drawing speed is too fast, the selection of blood collection point is improper, the tourniquet is used for too long, the blood collection vessel is not full, excessive shaking after blood collection, excessive vibration during transportation, etc. It can be subdivided into the following:
2.1 Specimen collection
Blood collection injury, such as repeated needle insertion and blood collection at hematoma; Collect blood from vascular access devices such as venous indwelling needle, infusion tube and central venous catheter; Syringe blood collection; Anterior median cubital vein, cephalic vein and basilic vein were not preferred; Use a fine needle; The disinfectant is not dry; Use tourniquet for more than 1 minute; Failing to mix in time and mixing violently; The blood collection volume is insufficient and does not reach the vacuum measurement scale of blood collection vessel; The quality of vacuum blood collection vessel and separating glue is poor; Use large volume vacuum blood collection vessels, etc.
2.2 Specimen transport
Violent vibration during pneumatic transmission; Long transit time; The temperature of the transfer vehicle is too high, violent vibration, etc.
2.3 Laboratory specimen processing& Hemolysis in vivo
Long preservation time of specimens; The preservation temperature of specimens is too high; Not centrifuged in time; Blood was not completely coagulated before centrifugation; The centrifugal temperature is too high and the speed is too fast; Re centrifugation, etc.
Autoimmune hemolytic, such as blood group incompatibility and blood transfusion; Genetic and metabolic diseases, such as thalassemia and hepatolenticular degeneration; Drug hemolytic reaction after medication, such as acute hemolytic reaction caused by intravenous injection of ceftriaxone sodium; Severe infection; Disseminated intravascular coagulation; Cardiac stent, artificial heart valve, extracorporeal membrane oxygenation, etc. The sample hemolysis caused by hemolysis in vivo shall not be rejected by the laboratory, and the doctor shall mark the description on the application form.
Post time: Apr-07-2022
